
Nearly a quarter of Medicare Advantage plans are providing nonmedical supplemental benefits this year, according to a new analysis by ATI Advisory. Nearly 1,300 MA plans are offering supplemental benefits this year — a 40% increase over the roughly 920 plans that offered them in 2021, the healthcare and aging services consulting firm found.
“There’s been a shift of [supplemental benefits] being something on the side that plans may not think much about,” Tyler Overstreet Cromer, principal at ATI Advisory, told McKnight’s Home Care Daily Pulse. “I think now every plan is thinking about how they can use these [benefits] to meet the needs of their members and grow market share.”
Increase in benefits for aging in place
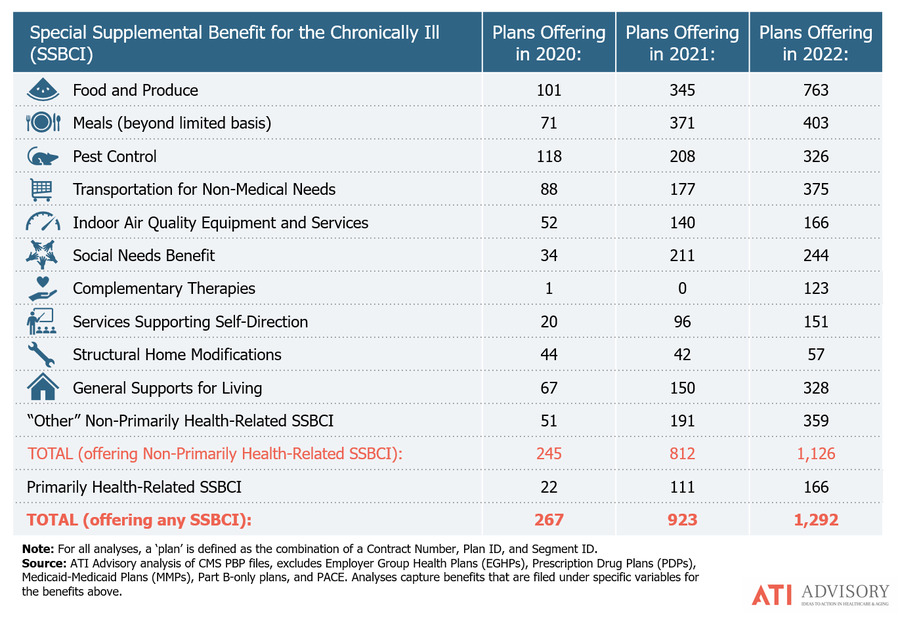
ATI Advisory found significant growth this year in MA plans offering benefits that help seniors age in place. Benefits such as food and meals, transportation, social needs and general supports for living all saw significant growth. Social needs benefits are services that address social isolation and loneliness. Supports for living benefits might include financial literacy and technology classes.
In 2019, the Centers for Medicare and Medicaid Services announced Medicare Advantage plans could begin offering special supplemental benefits for the chronically ill starting in 2020 that are not primarily health related. CMS intended the benefits to help MA plans tailor their offerings, so they could address gaps in care and improve health outcomes for the chronically ill.
More research needed
In the first year, fewer than 300 MA plans offered the supplemental benefits, but last year the number of plans offering them more than tripled. Still, there has been criticism that the insurance industry hasn’t done a good job educating seniors about the supplemental benefits their MA plans offer, and Cromer said there isn’t data yet on whether beneficiaries are taking advantage of the benefits.
ATI Advisory Analyst Elexa Rallos told McKnight’s Home Care Daily Pulse the insurance industry also needs to determine whether these benefits are saving payers money by reducing hospitalizations and emergency room visits and improving outcomes.
“We don’t think there has been enough evaluation yet in the field,” Rallos said. “We certainly think that will come later once the plans get their hands on how to deliver these [benefits].”



