
As the federal government sunsets pandemic-spurred Medicaid funding, states will be expected to foot the bill to keep Medicaid long-term services and supports (LTSS), which include home- and community-based services (HCBS), afloat.
An increase in the Federal Medical Assistance Percentage (FMAP), which provided enhanced federal Medicaid funding for states, is set to phase out next month as part of the Consolidated Appropriations Act of 2023. To make up for these lost funds, state Medicaid spending is projected to increase to more than 17% next year, according to a report by KFF.
While state Medicaid spending is projected to rise, total Medicaid spending is projected to fall. In FY 2022 and FY 2023, total Medicaid spending between states and the federal government grew to 9.8% and 8.3%, respectively, but 2024 will likely bring a sharp drop-off largely due to Medicaid disenrollment. The current “unwinding” period is expected to cause a net -8.6% Medicaid enrollment in FY 2024 — or up to 24 million individuals, according to the National Association for Home Care & Hospice. Of these, as many as thousands of home care patients could have already been affected by unwinding.
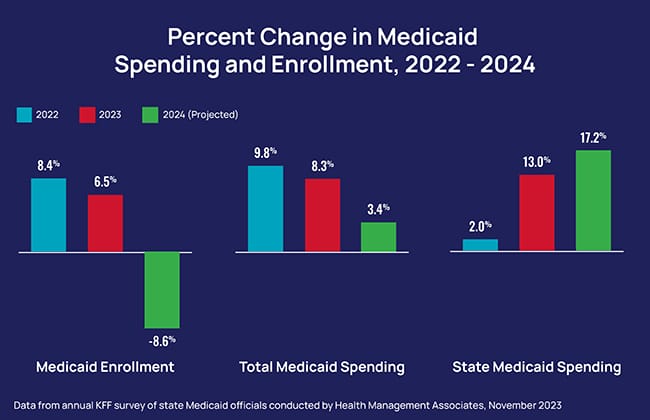
“For FY 2024, the total spending growth rate is projected to slow further, and the majority of states pointed to declines in enrollment during unwinding as the most significant downward pressure,” KFF noted.
Beyond enrollment growth, about half of the responding states cited provider rate increases as an upward pressure on spending in FY 2023 and FY 2024. Provider rate increases, inflation and workforce shortages leading to higher labor costs have also put pressure on states to spend more.
“Unwinding, macroeconomic uncertainties … and the loss of the enhanced FMAP and other expiring federal pandemic relief all add pressure and uncertainty to the Medicaid budgeting process, and by extension, to the state budgeting process,” KFF’s report noted. “Many Medicaid officials are therefore looking ahead cautiously knowing that they must be prepared to rapidly respond to worsening economic conditions, if and when they occur.”



